Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
Advertisement
Scientific Reports volume 13, Article number: 16345 (2023)
552
Metrics details
Assessment of morphometric and volumetric changes in lacrimal glands in thyroid eye disease, its clinical manifestations in relation of disease progression. Retrospective volumetric analysis included both genders and was performed on total of 183 patients – 91 patients with diagnosed Grave’s disease and thyroid eye disease and 92 patients without Grave’s disease and thyroid eye disease who underwent multidetector computed tomography (MDCT) examination in routine daily work according to other medical indications. In the group of females, there was statistical significance between patients with thyroid eye disease and controls who were smoking and had body weight gain. We found statistical significance in volumetric enlargements for both orbits in both genders for the patients group when compared to controls. There was also statistical significance in morphometric characteristics for the lacrimal gland diameters measured. Determination planimetric morphometric parameters of importance were coronary height of lacrimal gland of the right eye, coronary height of lacrimal gland of the left eye and coronary width of lacrimal gland of the left eye for the group of males. In a group of females the established determination parameters of importance were the coronary height of lacrimal gland of the left eye, the axial width of lacrimal gland of the left eye, volume of lacrimal gland of the right eye and the volume of lacrimal gland of the left eye. When we compared the displaced lacrimal gland coming forward (proptosis) in time progressing disease between group of patients and controls, we also found statistical significant connection. Evaluation of lacrimal gland volumetric and morphometric data may increase validity of defining this anatomical substrate and its morphology disruption as liable tool for thyroid eye disease progression follow up and treatment planning and outcome.
The lacrimal glands are paired amygdaloid glands located in the zygomatic process of frontal bone and specifically susceptible to autoimmune diseases such as Grave’s disease. Thyroid eye disease (TED), also known as Graves’ orbitopathy (GO) presents an autoimmune-driven ophthalmic clinical manifestation in Grave’s disease, and occurs primarily in patients with hyperthyroidism, but can also occur in patients with hypothyroidism and even euthyroidism. It can occur concurrently with endocrine abnormalities or may precede or follow them. Thyroid eye disease can induce periorbital oedema, erythema, proptosis, eyelid retraction, restrictive strabismus leading to diplopia, chemosis, and, in severe cases, increased intraocular pressure, exposure keratopathy, and even optic nerve compression. These symptoms might have serious physical and psychological consequences and impact the quality of life in many senses1. Thyroid eye disease may also have an impact on central nervous system function and cerebral cortical thickness inducing structural brain changes2. Displaced lacrimal gland coming forward and posterior herniation of the orbital fat are associated with optic neuropathy with a sensitivity of 94% and specificity of 91%3. Cigarette smoking is presumed to be the strongest risk factor for developing Grave’s orbitopathy4. Increased body weight and body mass index present also one of the risks for Grave’s orbitopathy and its complications5.
Currently, the disease is diagnosed using a combination of clinical signs and symptoms, laboratory tests, and imaging studies. MDCT is widely available, relatively inexpensive and highly reproducible testing methods of orbit at GO6. The progress assessment of TED and GO is determined by the Clinical Activity Score (CAS) by the presence or absence of seven inflammation signs or symptoms such as spontaneous retrobulbar pain, pain during movement of the eyes, redness of the eyelids, conjunctival redness, swelling of the eyelids, island lacrimalcaruncular lesions and conjunctival edema. CAS equal to 3 or greater suggests active GO7,8,9. Also, NOSPECS classification (No signs and symptoms, Only signs Soft tissue involvement, Proptosis, Extraocular muscle involvement, Corneal involvement and Sight loss), is used, which represents an ophthalmic mnemonic tool but with a lower use value10,11.
Computed tomography (CT) is a common imaging modality used in clinical practice for the diagnosis, treatment evaluation, and postoperative follow-up of thyroid eye disease. The use of Multi-detector row computed tomography (MDCT) in the diagnosis of GO enabled the production of large quantities of information in a relatively short time of the examination, but also a significant reduction of artifacts and errors in the measurement and evaluation of the orbital contents. Also, imaging software can reformat images in three planes (transaxial, coronary and sagittal) as well as high-resolution display images of orbital structures12. The quantitative relationship between the morphometric changes in lacrimal gland in patients with GO using planimetric and volumetric, morphometric analysis of orbital soft tissue presents no routine protocol so far13,14,15,16.
Our aim was to analyse and evaluate morphometric and volumetric characteristics of lacrimal glands in patients with thyroid eye disease by MDCT.
Retrospective volumetric analysis was done on 91 patients (19 males and 72 females aged from 18 to 80 with mean age 49.49 ± 12.02) diagnosed with Grave’s disease and TED. The patients included in this investigation were tested to TSH receptor antibodies by endocrinologist before MDCT examination. The study group patients included in this investigation had Graves’ disease coexisting with hyperthyroidism, hypothyroidism or euthyroidism by an endocrinologist. All study group patients were diagnosed de novo and there were no pharmacological treatment before our MDCT examination. Grave’s ophthalmopathy (GO) was considered to be present if eyelid retraction occurred in association with thyroid dysfunction, exophthalmos, extraocular muscle involvement or optic nerve disruption according to ophthalmologist as previously described17. We evaluated diagnostical volumetric and morphometrical radiological parameters but not therapeutical status of these patients.
The control group consisted of 92 patients (44 men and 48 women aged from 18 to 80 with mean age 52.15 ± 14.44) without Grave’s disease and TED. The control group of patients was formed based on the clinical picture and history. They were not TSH measured, because neither one patient included in control group did not have an endocrine disease or suspected endocrine disease, but was included by the method of random selection for the control group (underwent multidetector computed tomography examination in routine daily work according to other medical indications-sinusitis, headaches, ptosis, intracranial aneurysm, facial nerve paralysis, cranial nerve palsy). The inclusive parameter for entering the control group of patients was that they do not have thyroid disease, tumor or inflammation related to endocrine disease. The TSH receptor antibodies were not tested to control patients group nor was the TSH level determined.
All patients underwent MDCT examination of region of interest-orbit. MDCT examination of orbit was performed with 64-slice GE Healthcare LightSpeed VCT 64-slice CT Scanner scanner in routine 0.625 mm slice thickness endocranium protocol scanners. All examinations were performed MDCT natively first, followed by the intravenous administration of iodine contrast (Ultravist 300 mg/mL) in an amount of 50 mL, delayed 40 seconds.
Before the MDCT examination, an interview was conducted with all patients. Patients who were allergic to iodine contrast agent, had previous reaction to any contrast agent and/or antibiotic, had an increased risk of developing heart rhythm disorders, had previous had epileptic seizures, had impaired kidney and liver function in a short period before the MDCT examination, underwent MDCT of another region for another indication, which involved the use of an iodine contrast medium or were female patients pregnant or breastfeeding were not examined by MDCT in our investigation. After each of our MDCT examinations (study and control group), the patients were under 24-hour monitoring for any form of allergic reaction. No form of allergy to iodine contrast medium or any type of adverse reaction has been reported. In our study, we used Ultravist 300, which contains the active substance iopromide, which belongs to the group of nephrotropic low-osmolar X-ray contrast agents. Although the diagnostic recommendations for dosing Ultravist 300 iodinated contrast medium are 1-2 mL/kg of body weight, we conducted to all our patients a dose of only 50 mL, which in our clinical practice proved to be more than sufficient for examination and precise radiological computed tomography of orbit diagnostics. And in this way, we prevented and reduced the risk of “iodine-based contrast media-induced thyroid dysfunction”. It was shown that there is connection between immediate exposure to elevated iodide levels that can induce disruption of thyroid function and incident hyperthyroidism and hypothyroidism occurrence18,19,20,21. The Institutional Review Board of the University Clinical Centre of Serbia and Ethical Committee University Clinical Centre Medical faculty University of Belgrade approved this study (under number 29/IV-13).All participants need/requirement for informed consent was waived by ethical committee of the University Clinical Centre of Serbia Medical faculty University of Belgrade. All methods were performed in accordance with the relevant guidelines and regulations and informant consent was provided.
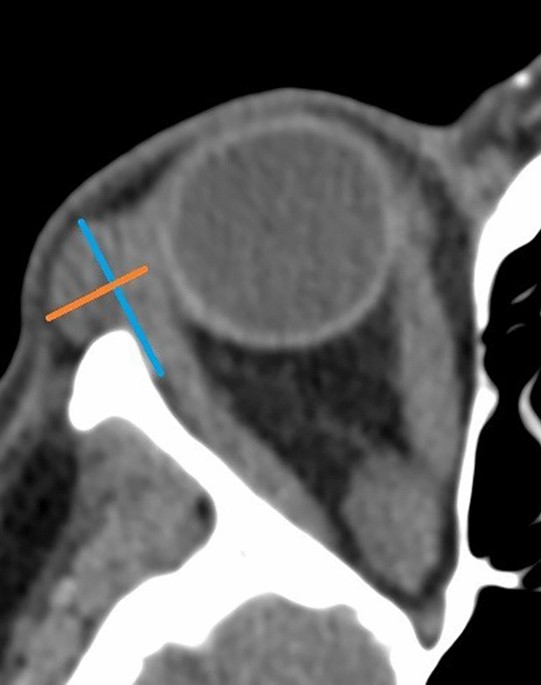
The volume rendering images of the lacrimal glands were obtained separately for the right (OD) and the left orbit (OS). Two neuroradiologists and one neuroscientist independently inspected MDCT scans. After interobserver evaluation agreement was agreed, the neuroscientist evaluated the remaining measurements. Volume rendering techniques (VRT) with MDCT allow excellent 3D reconstructions that help radiologists to visualize and analyse morphological anomalies in anatomical substrates as well as to evaluate their relation to other anatomical substrates and make specific treatment plans19,21. After using a tool for reorientation of DICOM images both axial and coronal images and volume dimensions of lacrimal glands were estimated. The MDCT parameters that were analyzed are lacrimal gland diameters (axial length, axial width, coronary height, and width) and volumes of the lacrimal gland (Figs. 1 and 2). Important parameter was if dislocated lacrimal gland coming forward, exophthalmos, proptosis, existed. In the examined axial image, the length was calculated from the most anterior point to the most posterior point of the gland and the width was calculated from the most lateral to the most medial point at the widest point perpendicular to the length at the same selected image slice. The examined anatomical substrate was delineated with a free hand technique by semiautomatic delineation tool in all consecutive images at the examined lacrimal gland. The volume of region of interest was calculated by the software 3D Slicer package. The results of 3D CT volume rendering images were compared with the axial images in order to calculate and test diagnostic sensitivity, specificity and accuracy.
Schematic view of the value of the axial length (marked in blue) and the axial width (marked in orange).
Schematic view of the value of coronary length, and high (marked in purple) and coronary width (marked in red).
Data analysis was performed using the method of descriptive analysis and exploratory analysis. Student t test was used to compare two independent groups. Pearson Chi-Square, odds ratio (OD) and relative risk (RR) were used to compare categorical parameters. Raw under the curve (ROC) was used for the level of sensitivity and specificity. The area under the curve (AUC) was used for testing the sensitivity of parameters. The cutoff point was defined as the positive/negative ratio (P/N ratio). Pearson correlation coefficient and coefficient of determination were used as a measure of linear association. Spearman correlation coefficient was used as a measure of association between scores. Significance was accepted at p<0.05. The power of tests was on level 80% or more. Data are presented as mean ± SD or median and range. Data analysis was done with SPSS v20.0 statistical software.
The Institutional Review Board of the University Clinical Centre of Serbia and Ethical Committee University Clinical Centre Medical faculty University of Belgrade approved this study (under number 29/IV-13). All participants need/requirement for informed consent was waived by ethical committee with full name. All methods were performed in accordance with the relevant guidelines and regulations and informant consent was provided.
Parameters included in this investigations were demographic, anthropometric (morphometric) and clinical (age, gender, smoking age experience, the number of cigarettes, body weight, height, body mass index (BMI), duration of disorders of thyroid function and duration of ocular signs).
Demographic characteristics are shown in Table 1. The results showed no statistical significance between patients with TED and controls in the group of males in demographic parameters. In the group of females, there was statistical significance between patients with TED and controls who were smoking. In the group of females there was a statistically significant difference between patients and controls expressed in a greater number of smokers in specific affected group p=0.000 (38 of 72; 53% of those affected in comparison to the control 5 of 48; 10%). There was statistical significance in the group of females related to weight for those with greater weight p=0.000 (72.72 +/– 7.14 kg in comparison to the controls 64.13 +/– 10.85 kg) and parameter BMI in which the group of patients had a higher BMI p=0.006 (27.12 +/– 5.2 kg/m2 when compared to controls 24.6+/– 4.1 kg/m2). Other parameters showed no statistically significant differences.
The morphometric and volumetric data analysis was conducted and obtained separately for the right and left orbit (Table 2, Figs. 1, 2).
There was statistical difference p = 0.002 (0.763 +/– 0.451 cm3 vs. 0.499 +/– 0.196 cm3) in a group of male patients and controls when volumes of the right orbits were compared as well as for the left orbits at the level of p = 0.039 (0.753 +/– 0.490 cm3 vs 0.497 +/– 0.181 cm3).
We also found statistical significance in a group of female patients and controls when volumes of the right orbits were compared p = 0.000 (0.735 +/– 0.250 cm3 vs. 0.521 +/– 0.250 cm3), and for the left orbits statistically significant difference was at the level of p = 0.000 (0.719 +/– 0.240 cm3 vs 0.554 +/– 0.245 cm3).
To determine the parameters of importance for the expression level of the disease, the multivariate binomial logistic regression was applied in a group of males. Determination planimetric morphometric parameters of importance were coronary height of lacrimal gland of the right eye (p = 0.001), coronary height of lacrimal gland of the left eye (p = 0.013) and coronary width of lacrimal gland of the left eye (p = 0.011) (Fig. 3).
Multivariate binomial logistic regression for estimation of the most important parameters for hazard ratio (Male). OD right orbit, OS left orbit.
Multivariate binomial logistic regression showed established determination parameters of importance, coronary height of lacrimal gland of the left eye (p = 0.007), the axial width of lacrimal gland of the left eye (p = 0.008), volume of lacrimal gland of the right eye (p = 0.048) and the volume of lacrimal gland of the left eye (p = 0.040) in a group of female patients (Table 3, Fig. 4).
Multivariate binomial logistic regression for estimation of the most important parameters for hazard ratio (Female).
The cutoff values for specific different parameters are showed with a ROC curve for both genders, female and male groups (Figs. 5 and 6).
ROC curve for the volumes of the right (OD) and left orbits (OS) in men.
ROC curves for the volumes of the right (OD) and left (OS) orbits in women. OD right orbit, OS left orbit.
All monitored parameters were statistically significant for determining the sensitivity and specificity (Table 4, Figs. 7 and 8).
ROC comparison between male and female patients (right orbit-OD).
ROC comparison between male and female patients (left orbit-OS).
When we compared the displaced lacrimal gland coming forward between group of patients and controls, we found statistical significant connection (p = 0.000). The sensitivity of displaced right lacrimal glands coming forward (OD) is 73.6%, while the specificity of 77.2%. Odds ratio was OR = 9.438 (4.810–18.521), and the relative risk of displacement, proptosis is RR = 3.226 (2.172–4.790) (Table 5).
When we compared the displaced lacrimal gland coming forward between group of patients and controls, we found statistical significant connection (p = 0.000). The sensitivity of displaced left lacrimal glands coming forward (OS) is 70.3%, while the specificity 78.3%. The odds ratio was OR = 8.533 (4.370–16.662), and the relative risk of displacement amounts to RR 3.235 (2.147–4.875) (Table 6).
Thyroid eye disease presents the most common extrathyroidal manifestation of Graves’ disease, autoimmune inflammatory disorder affecting the orbital tissues. Thyroid diseases occur generally more commonly in women than in men19,21. TED is not common, it occurs in a certain percentage of patients with Graves’ disease predominantly women. Our results also showed that persistence of left lacrimal gland displaced forward according to the diameters as more specific in women compared to males. In one of similar studies conducted, men demonstrated more asymmetric dynamics of disease like proptosis and overall asymmetry than women, while hyperthyroid females demonstrated more symmetry than euthyroid and hypothyroid males and females but in the same study, NO SPECS severity score was unaffected by gender, thyroid status, or symmetry. Greater sensitivity and specificity was observed in morphometric characteristics in left lacrimal glands in both gender showing potential in disease progression in our study. Previous investigations showed that the magnitude of lacrimal gland structural changes varied by gender emphasizing that the sexual dimorphism was most visible in men at all ages except pre-weaning and that male lacrimal tissue had considerably higher acinar area than females, which make important anatomical characteristics22. Previous animal studies has showed gender-related differences exist in lacrimal glands and that are correlated with morphological parameters of the lacrimal gland, as well as the volume, protein and IgG content of tears, measured in male and female infant, pre-weanling, pubertal, adult and old rats. In the same study, age-related variations occurred in the weight and morphological appearance of the lacrimal gland with the magnitude of structural changes dependent upon gender23. Clinical correlations with statistical significance conjoint with disrupted morphometric and volumetric data may pinpoint to disease progression in time. Our investigation showed statistical significance between patients with TED and controls who were smoking, number of cigarettes and greater body weight in the group of females. These findings are in the consistency with previous investigations that provided strong evidence for a causal association between smoking and development of TED. Smokers were also more likely to experience disease progression or poorer outcome of treatment. However, there were studies proving non correlation between smoking and TED, stating that there are no direct significant values correlating smoking habit to thyroid volume or function24. Results from a study conducted with smokers with Graves’ disease showed that they were more likely to experience rapid eye deterioration, including the development of double vision, the constriction of eye movement, and irreversible optic nerve damage25. On the other side, no statistically significant differences were observed in the body weight changes of hypothyroid and hyperthyroid patients, neither at diagnosis, nor following normalization of hormone levels after treatment in similar study26. Thyroid diseases generally occur more commonly in women than men27. Potential cause refers to the fact that thyroid dysfunction is associated with changes in body weight and composition, body temperature and total and resting energy expenditure independently of physical activity. Moreover, there is a fact that weight gain often develops after treatment of thyroid dysfunction. Obesity and thyroid dysfunction are common diseases, and consequently clinicians should be particularly alert to the possibility of thyroid dysfunction in obese patients and therefore correlation with TED28. Treatment of hyperthyroidism commonly results in weight gain, but the extent of weight gain is not well known, some of them may refer to psychological issues and psychiatric disorders. Patients may regain the weight they had lost or may overshoot and become obese29. The alteration of hormonal status may impact lacrimal glands morphology and function as well. Testosterone allows normal support and increased tissue proliferation of lacrimal glands, therefore chronic exposure to androgen receptor antagonists results in degenerative changes in lacrimal glands and volume reduction. According to previous investigations, estrogens’ role in anatomy of lacrimal glands is very debatable. While some researchers claim minimal invasiveness of estrogen in morphology of lacrimal glands others state adverse influence on the lacrimal gland, such as inducing glandular regression, acinar cell disruption, and necrosis30,31. Characteristic ophthalmic signs of TED that sometimes precede laboratory analysis include exophthalmos, eyelid retraction, eyelid oedema, restrictive extraocular myopathy, and optic neuropathy associated with thyroid dysfunction. Lacrimal gland presents anatomical substrate specifically affected in its volume and shape with emphasize on unilateral lacrimal gland enlargement which may present the predominate early clinical sign32. Our results showed both orbits alterations in volume and morphometric, planimetric characteristics in both genders. Also, when we compared the displaced lacrimal gland coming forward-proptosis between group of patients and controls, we found statistical significant connection in cases of both left and right lacrimal glands with slight greater statistical relevance in the case of left lacrimal gland. Lacrimal gland size and imaging characteristics are important since lacrimal gland may be defined as very significant anatomical, morphometric substrate and possible prognostic determinant in many specific diseases. Previous studies in the literature reported different sizes of lacrimal gland between different ethnicities. The first study which refers to lacrimal gland dimensions in healthy participant with CT showed significant difference only in mean coronal length between the right and left orbits, other dimensions were similar between two sides, compared to our results which showed significant results when it comes to the axial width of left lacrimal gland and coronal hights of both left and right lacrimal glands28,33.
Our investigation showed persistence of left lacrimal gland displaced forward according to the measured diameters as more specific in women with TED compared to males and its correlation with clinical data like smoking and obesity also more specific in females. MDCT structural imaging of lacrimal glands in patients with TED present a powerful diagnostic tool in clinical practice to diagnose and monitor the severity or progression of the disease along with other tests and examinations to help early diagnostics, treatment and managing TED. Volumetric and planimetric, morphometric lacrimal data correlate with statistical significance of clinical data making it possible morphological substrate for determination of Grave’s disease progression and dynamics and therefore MDCT routine scanning in conditions of medical indication presents a good pathway of observing and treatment modification of Grave’s disease. Future research with multiparametric CT imaging will improve the results by incorporating advanced post-processing techniques such as machine learning and texture analysis. A larger-scale multicentric study is needed to determine established dimensions of LGs that are representative of TED manifestation in both genders.
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Weiler, D. L. Thyroid eye disease: A review. Clin. Exp. Optom. 100, 20–25 (2017).
Article PubMed Google Scholar
Smith, T. J. & Hegedüs, L. Graves’ disease. N. Engl. J. Med. 375, 1552–1555 (2016).
Article PubMed Google Scholar
Giaconi, J. A., Kazim, M., Rho, T. & Pfaff, C. CT scan evidence of dysthyroid optic neuropathy. Ophthal. Plast. Reconstr. Surg. 18, 177–82 (2002).
Article PubMed Google Scholar
Kim, Sj. et al. Impact of smoking on thyroid gland: Dose-related effect of urinary cotinine levels on thyroid function and thyroid autoimmunity. Sci. Rep. 9, 4213. https://doi.org/10.1038/s41598-019-40708-1 (2019).
Article ADS PubMed PubMed Central CAS Google Scholar
Lu, C. et al. The relationship between obesity-related factors and graves’ orbitopathy: A pilot study. Medicina (Kaunas) 58(12), 1748. https://doi.org/10.3390/medicina58121748 (2022).
Article PubMed Google Scholar
Kirsch, E., Hammer, B. & VonArx, G. Graves’ orbitopathy: Current imaging procedures. Swiss Med. Wkly. 139, 618–23 (2009).
PubMed Google Scholar
Bartalena, L. et al. European Group on Graves’ Orbitopathy (EUGOGO): Consensus statement of the European Group on Graves’ orbitopathy (EUGOGO) on management of GO. Eur. J. Endocrinol. 158, 273–85 (2008).
Article PubMed CAS Google Scholar
Bartalena, L. & Tanda, M. L. Graves’ Ophthalmopathy. N. Engl. J. Med. 360, 994–1001 (2009).
Article PubMed CAS Google Scholar
Tachibana, S. et al. Orbital magnetic resonance imaging combined with clinical activity score can improve the sensitivity of detection of disease activity and prediction of response to immune suppressive therapy for Graves’ ophthalmopathy. Endocr. J. 5(7), 853–61 (2010).
Article Google Scholar
Dickinson, A. J. & Perros, P. Controversies in the clinical evaluation of active thyroid-associated orbitopathy: Use of a detailed protocol with comparative photographs for objective assessment. Clin. Endocrinol. (Oxf) 55, 283–303 (2001).
Article PubMed CAS Google Scholar
Soeters, M. R. et al. Optimal management of Graves orbitopathy: A multidisciplinary approach. Neth. J. Med. 69, 302–8 (2011).
PubMed CAS Google Scholar
Chapman, V. M., Grottkau, B. E., Albright, M., Salamipour, H. & Jaramillo, D. Multidetector computed tomography of pediatric lateral condylar fractures. J. Comput. Assist. Tomogr. 29, 842–6 (2005).
Article PubMed Google Scholar
Jung, W. S. et al. The radiological spectrum of orbital pathologies that involve the lacrimal gland and the lacrimal fossa. Korean J. Radiol. 8, 336–42 (2007).
Article PubMed PubMed Central Google Scholar
Fidor-Mikita, E. & Krupski, W. Computed tomography imaging of orbits in thyroid orbitopathy. J. Pre-Clin. Clin. Res. 2, 59–63 (2008).
Google Scholar
Soni, C. R. & Johnson, L. N. Visual neuropraxia and progressive vision loss from thyroid-associated stretch optic neuropathy. Eur. J. Ophthalmol. 20, 429–36 (2010).
Article PubMed Google Scholar
Fedorov, A. et al. 3D slicer as an image computing platform for the quantitative imaging network. Magn. Reson. Imaging 30(9), 1323–41 (2012).
Article PubMed PubMed Central Google Scholar
Bartley, G. B. & Gorman, C. A. Diagnostic criteria for Graves’ ophthalmopathy. Am. J. Ophthalmol. 119(6), 792–5. https://doi.org/10.1016/s0002-9394(14)72787-4 (1995).
Article PubMed CAS Google Scholar
Bednarczuk, T., Brix, T. H., Schima, W., Zettinig, G. & Kahaly, G. J. 2021 European Thyroid Association Guidelines for the management of iodine-based contrast media-induced thyroid dysfunction. Eur. Thyroid J. 10(4), 269–284. https://doi.org/10.1159/000517175 (2021).
Article PubMed PubMed Central CAS Google Scholar
Rhee, C. M., Bhan, I., Alexander, E. K. & Brunelli, S. M. Association between iodinated contrast media exposure and incident hyperthyroidism and hypothyroidism. Arch. Intern. Med. 172(2), 153–9. https://doi.org/10.1001/archinternmed.2011.677 (2012).
Article PubMed CAS Google Scholar
Avery, L. L., Susaria, S. M. & Novelline, R. A. Multidetector and three-dimensional CT evaluation of the patient with maxillofacial injury. Radiol. Clin. N. Am. 49, 183–203 (2011).
Article PubMed Google Scholar
Kavoussi, S. C., Giacometti, J. N., Servat, J. J. & Levin, F. The relationship between sex and symmetry in thyroid eye disease. Clin. Ophthalmol. 8, 1295–300. https://doi.org/10.2147/OPTH.S61041 (2014).
Article PubMed PubMed Central Google Scholar
Sullivan, D. A., Hann, L. E., Yee, L. & Allansmith, M. R. Age- and gender-related influence on the lacrimal gland and tears. Acta Ophthalmol. (Copenh.) 68(2), 188–94. https://doi.org/10.1111/j.1755-3768.1990.tb01902.x (1990).
Article PubMed CAS Google Scholar
Thornton, J., Kelly, S. P., Harrison, R. A. & Edwards, R. Cigarette smoking and thyroid eye disease: A systematic review. Eye (Lond.) 21(9), 1135–45. https://doi.org/10.1038/sj.eye.6702603 (2007).
Article PubMed CAS Google Scholar
Jastaniah, S. et al. Investigating the association of smoking with thyroid volume and function. Health 9, 1843–1851. https://doi.org/10.4236/health.2017.913133 (2017).
Article Google Scholar
Sawicka-gutaj, N. et al. Influence of cigarette smoking on thyroid gland—An update. Endokrynol. Pol. 65(1), 54–62. https://doi.org/10.5603/EP.2014.0008 (2014).
Article PubMed CAS Google Scholar
Tamboli, D. A., Harris, M. A., Hogg, J. P., Realini, T. & Sivak-Callcottet, J. A. Computed tomography dimensions of the lacrimal gland in normal caucasian orbits. Ophthal. Plast. Reconstr. Surg. 27, 453–56 (2011).
Article PubMed Google Scholar
Lee, J. S. et al. Computed tomographic dimensions of the lacrimal gland in healthy orbits. J. Craniofac. Surg. 24, 712–15 (2013).
Article PubMed Google Scholar
Bulbul, E., Yazici, A., Yanik, B., Yazici, H. & Demirpolat, G. Evaluation of lacrimal gland dimensions and volume in Turkish population with computed tomography. J. Clin. Diagn. Res. 10(2), TC06–TC08. https://doi.org/10.7860/JCDR/2016/16331.7207 (2016).
Article PubMed PubMed Central CAS Google Scholar
Ríos-Prego, M., Anibarro, L. & Sánchez-Sobrino, P. Relationship between thyroid dysfunction and body weight: A not so evident paradigm. Int. J. Gen. Med. 12, 299–304. https://doi.org/10.2147/IJGM.S206983 (2019).
Article PubMed PubMed Central Google Scholar
Sullivan, D. A. Tearful relationships? Sex, hormones, the lacrimal gland, and aqueous-deficient dry eye. Ocul. Surf. 2(2), 92–123. https://doi.org/10.1016/s1542-0124(12)70147-7 (2004).
Article PubMed Google Scholar
Gorimanipalli, B., Khamar, P., Sethu, S. & Shetty, R. Hormones and dry eye disease. Indian J. Ophthalmol. 71(4), 1276–1284. https://doi.org/10.4103/IJO.IJO_2887_22 (2023).
Article PubMed PubMed Central Google Scholar
Mulder, J. E. Thyroid disease in women. Med. Clin. N. Am. 82(1), 103–25. https://doi.org/10.1016/s0025-7125(05)70596-4 (1998).
Article MathSciNet PubMed CAS Google Scholar
Nawaz, S. et al. Computed tomography evaluation of normal lacrimal gland dimensions in the adult pakistani population. Cureus 12(3), e7393. https://doi.org/10.7759/cureus.7393 (2020).
Article PubMed PubMed Central Google Scholar
Download references
Laboratory for Multimodal Neuroimaging, Institute of Anatomy, Medical faculty, University of Belgrade, Belgrade, Serbia
Ana Starčević, Jovana Andrejic & Vuk Djulejic
Faculty of Organizational Sciences, University of Belgrade, Belgrade, Serbia
Zoran Radojičić
Center for Radiology, University Clinical Center of Serbia, Medical faculty, University of Belgrade, Belgrade, Serbia
Aleksandra Djurić Stefanović
Clinic for Otorhinolaryngology and Maxillofacial Surgery, University Clinical Center of Serbia, Medical faculty, University of Belgrade, Belgrade, Serbia
Aleksandar Trivić
Clinic for Neurosurgery, University Clinical Center of Serbia, Medical faculty, University of Belgrade, Belgrade, Serbia
Ivan Milić & Marina Milić
Clinic for Cardiology, University Clinical Centre of Serbia, Belgrade, Serbia
Dragan Matić
Faculty of Medicine, University of Belgrade, Belgrade, Serbia
Dragan Matić
Center for Radiology, Neurosurgery Clinic, University Clinical Center of Serbia, Medical faculty, University of Belgrade, Belgrade, Serbia
Igor Djoric
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
Conceptualization, A.S. and I.D.; Methodology, Z.R.; Software, A.S., J.A. and V.D.; Validation, I.D., A.T. and Z.Z.; Formal Analysis, M.I. and M.M.; Investigation, D.S.A.; Resources, I.D.; Data Curation, D.M.; Writing – Original Draft Preparation, A.S.; Writing – Review & Editing, A.S.; Visualization, A.S. and J.A.; Supervision, I.D.; Project Administration; Funding Acquisition, all authors contributed.
Correspondence to Ana Starčević.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
Reprints and permissions
Starčević, A., Radojičić, Z., Djurić Stefanović, A. et al. Morphometric and volumetric analysis of lacrimal glands in patients with thyroid eye disease. Sci Rep 13, 16345 (2023). https://doi.org/10.1038/s41598-023-43083-0
Download citation
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-43083-0
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Advertisement
© 2024 Springer Nature Limited
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.